Posted: July 25, 2024 | Author: Karin Verzijden | Filed under: Advertising, alternative protein, Authors, Enforcement, Food, Information |
 On 23 July 2024 a Dutch Court ruled in summary relief proceedings that Upfield cannot use the name “roombeter” for a plant-based alternative for butter, as this is in violation of the Regulation establishing a common organization of the markets for agricultural products (“COM Regulation”). You should know that “roombeter” translates in English as a composition of “cream” and “better”, whereas “cream” is a reserved designation under the COM Regulation that can only be used for dairy products. Furthermore, “beter” is close to “boter”, being the Dutch designation for butter.
On 23 July 2024 a Dutch Court ruled in summary relief proceedings that Upfield cannot use the name “roombeter” for a plant-based alternative for butter, as this is in violation of the Regulation establishing a common organization of the markets for agricultural products (“COM Regulation”). You should know that “roombeter” translates in English as a composition of “cream” and “better”, whereas “cream” is a reserved designation under the COM Regulation that can only be used for dairy products. Furthermore, “beter” is close to “boter”, being the Dutch designation for butter.
Facts of the case at hand
In the case at hand, Upfield markets a plant-based alternative for butter under the brand BLUE BAND and the product name ROOMBETER. The packaging of the product furthermore states “100 % plant-based alternative for butter” and “81 % less climate impact than butter”. The packaging itself consists of golden coloured paper that is also used for conventional butter in the Netherlands and it displays a curl of butter as shown below. The Dutch Dairy Association opposed the use of the product name ROOMBETER, as it is considered this a violation of the COM Regulation, as explained below.
Case before Dutch Advertisement Code Committee
Prior to this legal procedure , the Dutch Dairy Association had submitted a complaint regarding this product before the Dutch Advertisement Code Committee. This self-regulatory body ruled on March 21 last that the presentation of the product was misleading, since it could be understood to contain butter. The “e” in “beter” could be confused for an “o”, resulting in “boter”, which is Dutch for butter. And furthermore the golden coloured packaging added to the misleading character of the product. The topic of violation of the COM Regulation was left to civil law proceedings, as it exceeded the competence of the Committee.
Applicable legislation
Article 78.2 of the COM Regulation states that the definitions, designations and sales descriptions provided for in its Annex VII may be used in the Union only for the marketing of a product that conforms to the corresponding requirements laid down in that Annex. Annex VII contains, amongst other things, a product definition for milk and a list of milk products. It furthermore states that these designations may not be used for any other product than milk and milk products. The purpose of this provision is to protect dairy names from being used for non-dairy products.
Tofutown
You may recall that in its Tofutown decision back in 2017, the ECJ formulated a very strict prohibition of the use of diary names for non-dairy products (check out our blog on this case here). As a result of that prohibition, the use of the designation “Tofubutter” for a tofu-based product was in violation of the COM Regulation. As a general rule, the ECJ precluded the term ‘milk’ and the designations reserved by the COM Regulation exclusively for milk products from being used to designate a purely plant based product in marketing or advertising. This even applies if those terms are expanded upon by clarifying or descriptive terms indicating the plant origin of the product at issue
Arguments in favour of ROOMBETER
Upfield had argued it did not market its product under the designation ROOMBETER but under the designation BLUE BAND ROOMBETER. The brand BLUE BAND has been used for more than 100 years for margarine, so it is obvious for the consumer this is a plant-based product This is even strengthened by the Dutch translation of the designations “100 % plant-based alternative for butter” and “81 % less climate impact than butter”. So the name ROOMBETER does not designate, imply or suggest it is about a dairy product.
Court decision
The Court did not eat it. Instead, it very strictly applied the Tofutown doctrine, stating that a reserved designation under the COM Regulation cannot be used for a plant-based product. It went on to explain that if it is prohibited to use the designation “tofubutter” for a plant-based product, as it contains the reserved designation “butter”, for sure it is prohibited to use the designation “roombeter” for a plant-based product, as it contains another reserved designation under the COM Regulation. Also, the element “beter” (“better” in English) can hardly be perceived as a clarifying or descriptive term, as it does not refer (contrary to “tofu”) to a plant-based origin. In fact, its reference to plant-based origins can only be understood by those consumers who know the “skip the cow” ad or who further study the packaging of this product.
Upfield was therefore ordered to stop using the designation ROOMBETER within three months after the date of the legal decision.
Consequences of this decision
Should the conclusion of this decision be that any reference to dairy products should be meticulously avoided when marketing plant-based dairy replacements? This seems a very hard task, as manufacturers of these replacement products will want to indicate how their products can be used. Happily, this is not the case. It is still permitted to mention that your plant-based product is for instance a “yoghurt variation”, as this is perceived as a product explanation rather than a product designation. This is not in violation of the Tofutown doctrine and in line with a 2019 Dutch Supreme Court decision relating to a soy-based product marketed by Alpro. Advertising plant-based dairy alternatives nevertheless remains a delicate balancing act.
Posted: December 1, 2022 | Author: Jasmin Buijs | Filed under: Advertising, Enforcement, Food, Food Supplements, Health claims |
Intro
Food businesses operators that make medical claims for their products in the Netherlands can be fined for doing so under food law. However, they also run the risk of being fined under the Dutch Medicines Act (in Dutch: “Geneesmiddelenwet”), in which case much higher fine amounts apply. The latter sometimes provokes surprise and outrage. Based on three recent rulings, we see a positive trend, which is explained below.
Drug definition
 In principle, a medicinal product cannot be sold in the Netherlands without an authorization. Advertising a medicinal product that has not been authorized is prohibited as well. If a product is classified as such and sold without a license, the seller risks a hefty fine.
In principle, a medicinal product cannot be sold in the Netherlands without an authorization. Advertising a medicinal product that has not been authorized is prohibited as well. If a product is classified as such and sold without a license, the seller risks a hefty fine.
The legal definition of the term medicinal product and the corresponding authorization requirement can be found in the Dutch Medicines Act, which is based on the European Directive 2001/83/EC (the “Medicinal Product Directive”). The Medicinal Product Directive provides two criteria for the definition of a medicinal product: qualification by presentation and qualification by function. If a product meets one of these two criteria, it is classified as a medicinal product. The aforementioned criteria are further elaborated in case law.
Qualification by function
A product is a medicinal product by function (see the Hecht-Pharma judgment) if it can be administered to cure or prevent disease, diagnose or otherwise affect a person’s bodily functions. Of particular importance here are the composition and properties of the product, the method of use, the extent of distribution of the product, the consumers’ familiarity with the product and the health risks associated with its use.
Qualification by presentation
When applying the presentation criterion (see the Van Bennekom judgment), consideration is – unsurprisingly – given to whether a product should be regarded as a medicinal product on the basis of its presentation. It is not necessary that the product is expressly indicated or recommended as a medicinal product. The presentation criterion is already met if the manner of presentation gives the average consumer the impression that the product has a medicinal effect. The form in which the product is presented may give an indication for this, especially in the case of tablets, pills and capsules.
In particular the presentation criterion poses a risk to food companies. If they (unintentionally) make a medical claim in respect of their product, the presentation criterion may result in this product being classified (also) as a medicinal product by the Dutch Food and Consumer Product Safety Authority (“NVWA”). In that case, the NVWA may issue a fine under the Dutch Medicines Act. The starting point for such fine is €150,000, which is then differentiated based on the Policy rules of the Dutch Ministry of Health 2019. Even if the product also falls within the legal definition of food, the Dutch Medicines Act may apply simultaneously. The foregoing follows from the so-called hierarchy provision embodied in article 2.2 of the Medicinal Products Directive, which has been implemented into Dutch law as well. On the basis of this hierarchy principle, the Dutch Medicines Act is applicable if there is any doubt about the applicable product category. The result of this provision is that even a seller of coconut oil can receive a fine under the Dutch Medicines Act.
New trend in enforcement of medical claims?
Dutch case law gives numerous examples of products being classified as medicinal products by courts based on (solely) the presentation criterion. Recently, three court rulings have been rendered which give reason to assume that there is a new trend in case law. These are a ruling of the District Court of Oost-Brabant of March 25, 2022, and two (materially identical) rulings of the District Court of The Hague of June 28, 2022, regarding food supplements and follow-on milk, respectively.
The first case concerns the sale of dietary supplements, for which medical claims were made. The NVWA therefore classifies these supplements as medicinal products based on the presentation criterion and imposes two fines under the Dutch Medicines Act (both for sale and for advertising an unregistered medicinal product). The seller’s defense is that the Dutch Medicines Act should be interpreted in accordance with the Medicinal Product Directive and that it follows from there that the contested decision of the NVWA is based on an incorrect legal basis.
 The court agreed with this argumentation, referring to the amendment of the Medicinal Product Directive of 2004. The court deduces from the preamble to the amendment that the Medicinal Product Directive does not apply if there is no doubt that a product clearly exclusively belongs to another product category, such as food or food supplements. The court ruled that this was indeed the case for the specific circumstances that were under discussion. The products clearly fall under the category of food supplements and therefore solely food law applies. The court confirms that the Dutch Medicines Act must, after all, be interpreted in accordance with the Medicinal Product Directive. The court therefore does not proceed testing the medical claims made against the presentation criterion based on drug legislation at all.
The court agreed with this argumentation, referring to the amendment of the Medicinal Product Directive of 2004. The court deduces from the preamble to the amendment that the Medicinal Product Directive does not apply if there is no doubt that a product clearly exclusively belongs to another product category, such as food or food supplements. The court ruled that this was indeed the case for the specific circumstances that were under discussion. The products clearly fall under the category of food supplements and therefore solely food law applies. The court confirms that the Dutch Medicines Act must, after all, be interpreted in accordance with the Medicinal Product Directive. The court therefore does not proceed testing the medical claims made against the presentation criterion based on drug legislation at all.
Clearly food-only
The above ruling raises the question when a product is “clearly exclusively” a food and what aspects of the product are important in this respect. Indications for this can be found in the two recent decisions of the District Court of The Hague regarding specific food products for toddlers, namely follow-on formula. In its assessment of whether the follow-on formula in question could be a medicinal product by presentation, the court determined that such qualification is not obvious with regard to products sold in supermarkets and drugstores. Another factor in this case was that the detailed information about the follow-on formula, on the basis of which the Dutch Ministry of Health (the counterparty in the cases at stake) believed it to be a medicinal product by presentation, could only be found on the seller’s website.
Conclusion
Based on the rulings discussed, we signal a trend that judges are halting the current practice of enforcement of prohibited medical claims for food products based on the Dutch Medicines Act. The discussed rulings make clear that (prohibited) health claims for food supplements and for other food products such as follow-on formula should be assessed on the basis of the Food Information for Consumers Regulation (the “FIC Regulation”), and not via the presentation criterion based on the Dutch Medicines Act. In our opinion this is justified, because since the FIC Regulation became applicable, food law is specifically set up to do so. We are very curious to see whether the trend initiated above will be followed by other courts. Although it follows from a ruling of the District Court of Zeeland-West-Brabant of 21 October, 2022, that this is not yet the case, we trust this will only be a matter of time.
The above does however not mean that food business operators would be allowed to make medical claims for their products. Also, the FIC Regulation contains a ban on medical claims for food products and the Nutrition and Health Claims Regulation sets forth a strict regime for authorized health claims. Having said that, fines following a violation of food legislation are far lower than fines based on the Dutch Medicines Act. On balance, food companies are therefore better off with fines based on food legislation.
This blogpost is written by Max Baltussen, Karin Verzijden and Jasmin Buijs.
The authors want to acknowledge Ebba Hoogenraad and Irene Verheijen for sharing the case law discussed here.
Posted: October 25, 2021 | Author: Karin Verzijden | Filed under: Authors, Enforcement, Food |
 Over the last ten years, the trend of clean labelling in consumer food products has gained ever more ground. Clean labelling consists of replacing E numbers such as citric acid (E 330) and beetroot (E 162) by their natural counterparts, such as plant extracts. There is nothing wrong with E numbers per se. The use thereof is subject to specific purity criteria and their safety has been evaluated and approved. Consumers however tend to less appreciate E numbers as not being ‘natural’. This is not an unambiguous notion, as shown by this blogpost. Designing food products based on these consumer preferences can however become a tricky business, which was shown by a letter of the Dutch Ministry of Health, Welfare and Sport of 16 June this year as sent to the Dutch food industry associations. Even if this letter dates back to this Summer, it recently gained again traction on social media. We therefore consider it helpful to highlight the strict measures announced therein.
Over the last ten years, the trend of clean labelling in consumer food products has gained ever more ground. Clean labelling consists of replacing E numbers such as citric acid (E 330) and beetroot (E 162) by their natural counterparts, such as plant extracts. There is nothing wrong with E numbers per se. The use thereof is subject to specific purity criteria and their safety has been evaluated and approved. Consumers however tend to less appreciate E numbers as not being ‘natural’. This is not an unambiguous notion, as shown by this blogpost. Designing food products based on these consumer preferences can however become a tricky business, which was shown by a letter of the Dutch Ministry of Health, Welfare and Sport of 16 June this year as sent to the Dutch food industry associations. Even if this letter dates back to this Summer, it recently gained again traction on social media. We therefore consider it helpful to highlight the strict measures announced therein.
Fact-finding mission FVO in 2015
Some background information may be useful. In 2015, the Dutch Food Safety Authority NVWA received a visit from the Food and Veterinary office of the European Commission in the framework of a fact-finding mission. During this visit, non-authorised use of food additives in meat preparations was established that had not been detected by the Dutch authorities during official controls. After this visit, the NVWA announced the Action program on EU Food Additives (see paragraph 1.2 of this recent decision of the highest Dutch administrative law Appeal Court for further context). The Dutch Food Safety authority was thus confronted with its lack of oversight, which it clearly wanted to compensate.
NVWA published Additives Handbook in 2019
In June 2019, the NVWA published its Additives Handbook, which was updated in September 2020. The Additives Handbook also contains a chapter on clean labelling. In this chapter it is stated that the use of plant extracts in consumer food products, that are merely applied for their technological function, should be regarded as unauthorized use of additives. An example is beetroot extract containing high levels of nitrate that can be converted into nitrite for use in meat preparations. The converted nitrite is identical to the additive nitrite, except that it does not necessarily meet the additives purity criteria. The PAFF Committee also considers that such cases represent targeted use of food additives, because the plant extracts at stake are merely used for their technological function, such as preservative, antioxidant or colorant. This use of plant extracts should therefore meet all applicable criteria to food additives, including being authorized as such. To easily verify which additives can be used in which foods and under which conditions, the NVWA also recently launched an interactive tool on its website.
Health Ministry’s letter of 6 June 2021
This Summer’s letter of the Dutch Ministry of Health, Welfare and Sport (in consultation with the NVWA) is even more concrete. It announces active enforcement regarding the unauthorised use of additives, as set out above, which it also considers as misleading information for consumers. As an additional example, the letter also states the use of microcultures, that are mainly used because of their preservative function. Enforcement measures can be avoided when four cumulative conditions have been met:
- an application for the clean label ingredient at stake as an authorised additive has been filed to the European Commission, who has confirmed the application is complete;
- the application was done before 1 January 2022;
- the clean label ingredient at stake has been used in food products since 16 June 2021 or before;
- the declaration of the clean label ingredient at stake includes its technological function.
Consequences of the Health Ministry’s letter
The letter of the Dutch Ministry of Health, Welfare and Sport in fact introduces a (very short) transition regime for food business operators using plant extracts and other ‘clean label ingredients’ mainly for their technological function in food products sold to consumers. These companies have two options. The first one is to make the investment for an application regarding an authorised additive in due course and revising their product labels as set out above (i.e. specification of the technical function of the clean label ingredient). This is for sure a costly and lengthy option, so it may be worthwhile to make such application on an industry level, as authorisations are generic. This is however only a viable option when the clean label ingredient was already used in food products for its technological function on or prior to 16 June of this year. The second option is to reformulate their product by using the ‘conventional’ additives and mentioning the appropriate E numbers on their product labels. In case neither option is retained, it follows from the NVWA’s food information intervention policy that a written warning can be triggered, followed up by a fine if the warning does not result in compliance. If and when any such warning is received, it should of course be meticulously studied if the correct legal basis was cited and if indeed a warning logically follows therefrom. If not, an administrative complaint before the NVWA can be lodged in first instance and an administrative appeal in second instance. We expect to see a lot of these in the near future if clean label enforcement will be as tight as announced in the letter of 16 June of this year.
Posted: January 11, 2021 | Author: Karin Verzijden | Filed under: Authors, Enforcement, Food, Food Supplements, Nutrition claims |
 Introduction
Introduction
Last week I received a call from an entrepreneur who wanted to know what requirements he had to bear in mind when distributing food supplements from Finland to other EU Member States. I told him about the language requirements for mandatory food information. I also informed him that the allowed level of vitamins and minerals could differ from Member State to Member State. Furthermore, in some countries a so-called notification system for market access has been put in place, whereas in others, no such system applies. Finally, I informed him that there is no harmonised approach on prohibited substances in the EU either. In fact, he was quite surprised to learn about all this, as he thought food supplements to be subject to the principle of free circulation of goods in the internal market. Is not that correct? Yes, it is. However, as follows from the above, a number of exceptions apply to this principle. This blogpost explains what is being done to achieve more harmonisation in the food supplements market.
Food supplements: what are they in fact and what happens in practice?
According to the Food Supplements Directive, food supplements are meant to supplement the normal diet. They are concentrated sources of nutrients or other substances having a nutritional or physiological effect that are mostly sold in the form of pills or powders. While nutrients are vitamins and/or minerals, such other substances are, for example, amino acids, glucosamine or certain substances contained in herbs or plants. What we see in practice, is that more and more consumers use food supplements not only to supplement their diet, but for a targeted health effect. Increasing concentration or improving sport achievements are two examples thereof. Another trend is that a broad number of food supplements is nowadays offered for sale online. As many of them come with striking health claims, it is not always sufficiently clear for consumers what they are actually buying. In these COVID-times, many supplements claimed for example to boost the immune system without meeting the specific requirements for such claim. This may create a dangerous situation if and when dangerous substances are involved.
Food supplements: a boosting market but not without risks
The market of food supplements in the Netherlands alone was valued in 2019 by Neprofarm at € 143 million. In that same year, the Netherlands pharmacovigilance centre Lareb received 165 notifications of adverse reactions regarding food supplements. Even worse, the Netherlands Intoxications Information Centre NVIC reported 891 cases of intoxications through the use of food supplements in 2019. These adverse effects or intoxications may result in stomach complaints, headaches or dizziness, but also in more severe conditions such as hart complaints or even cerebral haemorrhage. It follows from inspection results of the Dutch Food Safety Authority NVWA that only 45 % of the food business operators comply with all applicable food safety requirements. Due to the lack of regulatory harmonisation in this field and the open norm laid down in the General Food Law Regulation (article 14 thereof states “food shall not be placed on the market if it is unsafe”), this makes effective enforcement of food safety for food supplement a complex task.
Dutch initiatives aimed at more EU harmonization for food supplements
In an ideal world, dangerous substances are prohibited on an EU-wide basis. Currently, an initiative is ongoing to add substances to the list of unsafe substances under the Fortification Directive. Furthermore, in February 2020, an initiative was launched by the enforcement authorities of 18 Member States including those of the Netherlands, to draft a joint list of prohibited substances for food supplements. Since both initiatives are not expected to materialize overnight, the Dutch Health Minister has decided, in cooperation with the Dutch Food Safety Authority and the Dutch Medicines Evaluation Board CBG amongst others, to draft a national list of unsafe substances. This list will be based on risk evaluations pertaining thereto and the aim is to give this list a statutory basis, by integrating it in the Dutch Commodities Act (“Warenwet”). Furthermore, the Dutch Food Safety Authority has designed a targeted approach of sales of food supplements via the internet. Based on the Dutch polder tradition, this approach is consensus-based, aiming to agree with online marketplaces that they remove from their offerings any food supplements containing prohibited substances. Also, the Dutch Health Minister oversees that the communications to consumers on food supplements by a number of channels, such as the Netherlands Nutrition Centre (“Voedingscentrum”), the Health Inspectorate IGJ and the National Institute for Public Health RIVM, provides proper risk information. Finally, the Health Minister considers introducing a system of prior notification and some level of safety evaluation into the Netherlands as well.
Are these initiatives a good thing or a bad thing?
In order to enhance consumer safety, the above initiatives are certainly a good thing. For food business operators however, they may entail further obstacles to the free circulation of goods in the internal market. Based on the new Official Controls Regulation, enforcement authorities are allowed to do “mystery shopping”, i.e. ordering food supplements without identifying themselves. Once the Dutch national list of dangerous substances will have a statutory basis, the Dutch Food Safety Authority could do online test purchases with EU food business operators that may not be aware of such list. If their products are not in line therewith, they are subject to enforcement measures. As to the intended introduction of the notification requirement of food supplements in the Dutch market, this will certainly make market access less smooth.
On the other hand, in a number of EU countries, such as Belgium and France, a system of prior notification for food supplements is already in place. In practice, we see this can operate as a “safety seal”, meaning that supplements that were allowed on those markets, potentially earn more easily market access in other Member States as well. Furthermore, a new tool is available to food business operators since the new Regulation on mutual recognition became applicable in April 2020. Article 4 thereof offers the possibility to draw up a voluntary declaration to demonstrate to the competent authorities of other Member States that a food product is lawfully marketed, for instance in the Netherlands. The competent authorities in the Member State of destination can only oppose the further marketing thereof based on legitimate public interest, for instance public health. I expect this to be as useful tool for the further circulation of food supplements in the internal market.
Finally, I expect the Dutch national list of unsafe and hence prohibited substances for food supplements also to provide some more clarity in this field, provided that it will also be easily accessible to food business operators abroad. When these food business operators indeed duly inform themselves, this list could facilitate the successful EU-wide launch of food supplements, with less unclarity pre-launch and less surprises after launch. Which is supposed to be a good thing.
The information shared in this blogpost stems from a letter of the Dutch Health Minister to the Dutch House of representatives dated 14 December 2020, which can be viewed here (in Dutch only).
Posted: October 2, 2020 | Author: Jasmin Buijs | Filed under: Authors, cannabidiol, cannabis, Disclosure of information, Enforcement, Food, Food Supplements, Health claims |
 Since 1 September 2020, the Dutch Food Safety Authority (NVWA) has been given the power to publish certain inspection results (including identification details of the inspected FBO) faster than before. Prior to that date, the legal basis for disclosure could primarily be found in article 8 of the Dutch Freedom of Information Act (in Dutch: Wet openbaarheid van bestuur). This act creates a duty for the administrative body concerned, for example the NVWA, to publicly provide information when this is in the interest of good and democratic governance. However, article 10 of the Freedom of Information Act requires an individual balancing of interests in order to avoid disproportionate disadvantage for the parties involved as a result of the publication. It also prohibits disclosure of certain sensitive information, such as company and manufacturing data that has been confidentially communicated to the government. This blog post explains what has changed since 1 September 2020, which FBOs are affected and what arguments they can use to prevent disclosure.
Since 1 September 2020, the Dutch Food Safety Authority (NVWA) has been given the power to publish certain inspection results (including identification details of the inspected FBO) faster than before. Prior to that date, the legal basis for disclosure could primarily be found in article 8 of the Dutch Freedom of Information Act (in Dutch: Wet openbaarheid van bestuur). This act creates a duty for the administrative body concerned, for example the NVWA, to publicly provide information when this is in the interest of good and democratic governance. However, article 10 of the Freedom of Information Act requires an individual balancing of interests in order to avoid disproportionate disadvantage for the parties involved as a result of the publication. It also prohibits disclosure of certain sensitive information, such as company and manufacturing data that has been confidentially communicated to the government. This blog post explains what has changed since 1 September 2020, which FBOs are affected and what arguments they can use to prevent disclosure.
Additional basis of disclosure as of 1 September 2020
As of 1 September 2020, the NVWA is additionally bound by the Decree on the Disclosure of Supervision and Implementation Data under the Health and Youth Act (in Dutch: Besluit openbaarmaking toezicht- en uitvoeringsgegevens Gezondheidswet en Jeugdwet, hereinafter: Decree on Disclosure), as further elaborated in the Policy Rule on Active Disclosure of Inspection Data by the NVWA (in Dutch: Beleidsregel omtrent actieve openbaarmaking van inspectiegegevens door de NVWA, hereinafter: Policy Rule on Disclosure). This power of disclosure is based on article 44 of the Dutch Health Act (in Dutch: Gezondheidswet). Disclosure in accordance with the Decree on Disclosure does not require the balancing of interests: disclosure of information will simply take place when indicated in the relevant annex to the Decree on Disclosure. Companies that wish to prevent publication of information related to their business will therefore have to invoke factual criteria, such as that the information to be disclosed contains incorrect information or concerns information that is excluded from disclosure in Article 44(5) of the Health Act.
Required actions when companies disagree with disclosure
The publication of information as based on the Decree on Disclosure has consequences for the way affected companies can stand up to prevent disclosure and the speed with which they will need to object. Where the Freedom of Information Act offers affected companies the possibility to share their opinion (in Dutch: zienswijze) in reaction to the administrative body’s intention to disclose the information in question, this possibility does not exist under the Decree on Disclosure. If and when an affected company does not agree with disclosure on the basis of the latter decree, this company has two weeks to object to the respective administrative body’s intention of disclosure and needs to seek interim relief measures within this time frame in order to actually suspend the disclosure. In addition, under the Decree on Disclosure companies are provided the option to write a short response that will be published together with the information subject to disclosure. In this way, affected companies are given the opportunity to provide the outside world with a substantive (but very summary) response to the information to be made public. The Policy Rule on Disclosure in fact also grants this right of response to information disclosed by the NVWA under the Freedom of Information Act.
Relevant for all FBOs?
The aforementioned additional legal basis for disclosure by the NVWA applies for the time being to a limited number of supervisory areas only, namely the inspection results of the NVWA with regard to (i) fish auctions, (ii) the catering industry, and (iii) project-based studies into the safety of goods other than food and beverages. These areas may be expanded in the future, according to the explanatory notes to the Decree on Disclosure.
 However, for companies with so-called borderline products that navigate between different regulatory regimes, it is relevant to know that Dutch Health and Youth Care Inspectorate (IGJ) has broader powers to actively disclose inspection results under the Decree on Disclosure. Since 1 February 2019, the IGJ has already been publishing information on the basis of this decree regarding, amongst other, compliance with the Dutch Medicines Act (in Dutch: Geneesmiddelenwet). This means that when the IGJ takes enforcement measures against a FBO handling food supplements or other foodstuffs that qualify as (unregistered) medicines, it may be obliged to make public the respective supervisory information. The same applies to enforcement under the Dutch Medical Devices Act (in Dutch: Wet op de medische hulpmiddelen) – think diet preparations – and the Opium Act (in Dutch: Opiumwet) – think CBD and other cannabis products.
However, for companies with so-called borderline products that navigate between different regulatory regimes, it is relevant to know that Dutch Health and Youth Care Inspectorate (IGJ) has broader powers to actively disclose inspection results under the Decree on Disclosure. Since 1 February 2019, the IGJ has already been publishing information on the basis of this decree regarding, amongst other, compliance with the Dutch Medicines Act (in Dutch: Geneesmiddelenwet). This means that when the IGJ takes enforcement measures against a FBO handling food supplements or other foodstuffs that qualify as (unregistered) medicines, it may be obliged to make public the respective supervisory information. The same applies to enforcement under the Dutch Medical Devices Act (in Dutch: Wet op de medische hulpmiddelen) – think diet preparations – and the Opium Act (in Dutch: Opiumwet) – think CBD and other cannabis products.
 An example: melatonin-containing foodstuff labeled as a medicine
An example: melatonin-containing foodstuff labeled as a medicine
An example of a FBO that was faced with disclosure in accordance with the Decree on Disclosure by the IGJ concerns a company involved in melatonin-containing products. The IGJ intended to publish an inspection report on these products, from which it would follow that the products in question qualify as medicines and that the FBO concerned would therefore illegally place them on the market (namely without the required licenses under the Medicines Act). The FBO at stake applied for a preliminary injunction suspending the publication decree. On 8 July 2020, the preliminary relief judge rendered a judgment in this case.
Possible factual criteria to prevent naming & shaming
Although disclosure under the Decree on Disclosure is obligatory and disclosure decisions thus do not require the balancing of interests, the above-mentioned melatonin case gives good insights into the factual criteria that can nevertheless be invoked to prevent disclosure. In this case, the respective FBO brought forward the following arguments.
The respective inspection report excluded from disclosure
Article 3.1(a) of Part II of the Annex to the Decree on Disclosure excludes certain supervisory information from disclosure, including the results of inspections and investigations established as a result of a notification by a third party. The FBO at stake (hereinafter: “Applicant’) takes the position that the present inspection report was initiated as a result of a notification or enforcement request by a competitor. This would mean that the respective inspection report must not be made public.
The preliminary relief judge cannot agree with this position in the present case and rules that the inspection report is clearly related to an earlier letter from the IGJ to the applicant in which it announced the intensification of supervision of melatonin-containing products. Moreover, the case file was silent on a notification or enforcement request by a competitor.
The preliminary relief judge additionally states that it agrees with the IGJ’s viewpoint that the inspection report does not concern a penalty report (the report was drafted within the context of supervision and only indicates that Applicant will be informed about the to be imposed enforcement measure by separate notice). The fact that Applicant had earlier received a written warning for violation of the Medicines Act has no influence on this. The inspection report is therefore neither excluded from publication pursuant to article 3.1(a)(ii) of Part II of the Annex to the Decree on Disclosure, which makes an exception for “results of inspections and investigations that form the basis of decisions to impose an administrative fine”.
Disclosure in violation of the goal of the Health Law: outdated scientific foundation conclusions IGJ
The purpose of disclosure under the Health Act, in the wording of article 44(1) of that act, is to promote compliance with the regulations, to provide the public with insight into the way in which supervision and implementation of the Decree on Disclosure is carried out and into the results of those operations. Pursuant to Article 44a(9) of the Health Act, information should not be made public where this is or may violate aforementioned purpose of disclosure. Applicant takes the position that publication of the present inspection report does not contribute to improved protection of the public or to better information about the effects of melatonin, as a result of which the report should not be disclosed. More specifically, the applicant complains that the report (i) contains obvious errors and inaccuracies, (ii) gives the impression that it concerns a penalty decision, and (iii) is based on an incorrectly used framework to determine whether the qualification of a medicine is met.
The preliminary relief judge first of all notes that the fact that Applicant does not agree with the conclusions of the inspection report does not mean that the report therefore contains obvious inaccuracies. The preliminary relief judge further summarizes Applicant’s position as follows: (i) the IGJ wrongly took a daily dosage of 0.3 mg melatonin to determine the borderline between foodstuff and medicines; (ii) in doing so, the IGJ did not demonstrate that products with a daily dose of 0.3 mg melatonin actually acts as a medicine; (iii) moreover, the product reviews refer to outdated scientific publications (a more recent study by one of the authors thereof as well as more recent EFSA reports have not been included in the inspection report), whereas the current state of scientific knowledge must be taken into account according to established case-law. For these reasons, the preliminary relief judge agreed with Applicant that the IGJ has not made it sufficiently clear that from a daily dose of melatonin of 0.3 mg or more a ‘significant and beneficial effect on various physiological functions of the body’ occurs scientifically – according to the current state of scientific knowledge – and that products with a daily dose of melatonin of 0.3 mg or more act as a medicine”. Having said that, the preliminary relief judge did not accept Applicant’s statement that disclosure is contrary to the purpose of disclosure under the Health Act. Instead, the preliminary relief judge sought to comply with the so-called principles of sounds administration (in Dutch: algemene beginselen van behoorlijk bestuur) and ruled that the disclosure decision was not diligently prepared and insufficiently substantiated.
Incorrect facts
Applicant claims that the inspection report contains various inaccuracies, including the incorrect information that Applicant would produce melatonin itself. Applicant had already raised these inaccuracies in her response to the draft version of the report, but this had not resulted into adjustments in the final, to be published version of the report. The preliminary relief judge ruled on this matter that the IGJ should further investigate Applicant’s concerns and should amend the report where relevant. After all, the content of the report must be correct and diligently compiled. The mere fact that Applicant was given the opportunity to respond to the draft version of the report and that the IGJ responded to this in its decision to disclose the report does not mean that this requirement is met.
Violation of article 8 ECHR: disclosure has a major impact on Applicant’s image
Applicant claims that the planned disclosure will have a major impact on Applicant’s image and that of the natural person involved in the company. This is in violation of article 8 of the European Convention on Human Rights (ECHR) concerning the right to respect for private and family life. The Explanatory Memorandum to the Amendment to the Health and the Youth Care Act (in Dutch: Memorie van Toelichting op de Wijziging van de Gezondheidswet en de Wet op de Jeugdzorg) deals with this in detail. It emphasizes that the disclosure of inspection data does normally not constitute an interference with private life, because the data normally relates to legal persons and not to natural persons. The aforementioned Explanatory Memorandum therefore concludes that article 8 ECHR does not preclude disclosure on the grounds of the Health Act. Nevertheless, the court has at all times the competence to review a disclosure decision in the light of that article, in which case it will in fact have to balance the interests involved. In the present case, preliminary relief judge sees however no reason to assume a violation of article 8 ECHR.
Although the above shows that the preliminary relief judge in the respective melatonin case does not agree with all arguments put forward by Applicant, the request for suspension of publication of the contested inspection report was nevertheless granted thanks to factual criteria that were sufficiently substantiated. In particular the (implicit) argument that the conclusions in the inspection report lack a sufficient factual basis affects the essence of the information to be disclosed.
Conclusion
Rapid action is required to prevent active disclosure of inspection results under the Decree on Disclosure as these will usually be published after two weeks. This is not only relevant for FBOs active in the supervisory areas of the NVWA as designated in the Decree on Disclosure, but also for FBOs that operate at the interface of legal regimes under the supervision of the IGJ. To suspend disclosure, interim relief proceedings will have to be instituted as the Decree on Disclosure no longer provides for the possibility of submitting an opinion prior to publication. Moreover, affected companies cannot invoke the argument of suffering a disproportionate disadvantage as a result of the publication. Publication on the basis of the Decree on Disclosure is namely not subject to an individual balancing of interests (apart from an assessment on the basis of article 8 ECHR, insofar relevant). Although the arguments that companies can bring forward to prevent publication are therefore more limited than in the case of disclosure under the Freedom of Information Act, this does not mean that companies cannot successfully object an intention of disclosure. The melatonin case mentioned above is an example of this: conclusions that are not based on most recent science may not be published without adequate justification. Also, facts that are alleged to be incorrect should be further investigated before disclosure.
Posted: February 25, 2019 | Author: Karin Verzijden | Filed under: Authors, cannabidiol, cannabis, Enforcement, Food, Health claims, novel food |
 Recently, CBD food products were qualified as Novel Foods requiring a market authorization. The lively trade in these products therefore currently seems to be at risk. However, not all cannabis derived products are Novel Foods. What is the current state of play regarding these products and how is enforcement going to look like?
Recently, CBD food products were qualified as Novel Foods requiring a market authorization. The lively trade in these products therefore currently seems to be at risk. However, not all cannabis derived products are Novel Foods. What is the current state of play regarding these products and how is enforcement going to look like?
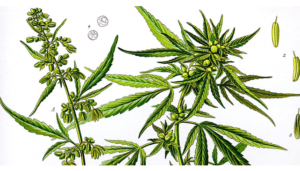
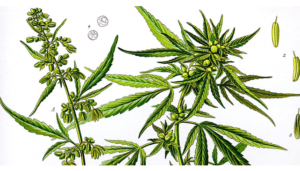
Current state of play re. cannabis derived products
In the European Union, the cultivation of Cannabis sativa L. varieties is permitted provided they are registered in the EU’s ‘Common Catalogue of Varieties of Agricultural Plant Species’ and the tetrahydrocannabinol (THC) content does not exceed 0.2 % weight per weight. The Common Catalogue is embodied in the EC Plant Variety database, which currently lists 68 species of Cannabis sativa. Some products derived from the Cannabis sativa plant or plant parts such as seeds, seed oil, hemp seed flour and defatted hemp seed have a history of consumption in the EU and therefore, in principle, are not novel.
What’s new?
This is different for extracts derived from Cannabis sativa L. and derived products containing cannabinoids, such as cannabidiol (CBD). It follows from a recent clarification of the Novel Food Catalogue that these products are considered Novel Foods, as a history of consumption regarding these products has not been demonstrated. This applies to both the extracts themselves and any products to which they are added as an ingredient. If for instance CBD is added to hemp seed oil, the product can no longer be marketed just like that and requires market authorization. The status of Novel Food also applies to extracts of other plants containing cannabinoids and to synthetically obtained cannabinoids.
How does the market of CBD food products currently look like?
Currently, the market in CBD food products is flourishing. A variety of CBD nutraceutical products is being offered for sale, such as HempFlax CBD, CBD oil, but also CBD-infused tea, honey or sweets. Although there is no hard-scientific evidence, many health benefits are connected to CBD food products, such as stress reduction, good night rest and providing energy and increasing resistance. Contrary to products containing THC (tetrahydrocannabinol), which is also extracted from cannabis, you do not get high on CBD food products, as this is not a psychoactive substance.
Medicinal use of cannabis
The use of cannabis derived CBD in food is not to be confused with medicinal use of cannabis. In most cases of medicinally applied cannabis, the active ingredient is THC, not just CBD, or a combination of THC and CBD. Although medicinally applied cannabis does not play a role in the cure of diseases, scientific publications show it can alleviate suffering from diseases, for instance nausea, decreased appetite, slimming or weakening due to cancer.
Consequences for business of the change in legal framework
Due to the qualification of CBD food products as Novel Foods, the lively trade in these products is currently at risk. Any Novel Food has to obtain a market authorization in order to get market access. CBD food products currently marketed may face enforcement measures, unless they can benefit from the transition regime laid down in the Novel Foods Regulation. According to this transition regime, any product that did not fall within the scope of the former Novel Foods Regulation, was lawfully marketed prior to 1 January 2018 and for which an application for market authorization is filed before 2 January 2020, can continue to be marketed until an authorization decision has been taken. While this transition period is in principle drafted for Novel Foods that fall into one of the new novel food categories under the new Novel Foods Regulation, it is in the spirit of the transition regime to also include the CBD scenario.
Pending CBD-application and expected EFSA opinion
Currently, one application for the authorization of a CBD food supplement is pending. The application was made by the company Cannabis Pharma from the Czech Republic and is based on publicly available safety and toxicological information and toxicity reviews. More in particular, the scientific data has been gathered from acute and long-term toxicity studies in animals and tolerance studies in humans. The data package submitted aims to support the safety of the use of CBD in food supplements for adults with a daily intake of up to 130 mg or 1.86 mg/kg body weight. It is reported by various sources that an EFSA opinion is awaited this March (see here and here).
Any benefits for the CBD market of a positive EFSA opinion?
Contrary to the situation under the former Novel Foods Regulation, the authorizations granted under the current Regulation have a generic nature. This means that any other company meeting the conditions of use stated in the authorization, would be at liberty to market CBD food supplements as well. The pending application made by Cannabis Pharma is therefore followed with great interest by the CBD market. As they do not seem to rely on data protection, a granted authorization would pave the way for other food supplement companies. It is not certain if this will happen still this year. If and when EFSA grants a positive opinion this March, the European Commission still has 7 months to submit an implementing act to the PAFF Committee. Upon a positive opinion of the PAFF committee, such implementing act could be quickly adopted. If the PAFF Committee has no opinion or a negative opinion, 1 or 2 months should be added to the procedure as a minimum.
Ireland: some CBD food products can be marketed
Meanwhile, there is some guidance available at Member State level. The Irish Food Safety Authority notes that recently a large number of CBD food products entered the market, typically marketed as food supplements in liquid or capsule form. Depending on the manufacturing process applied, the trade in CBD oil is not prohibited, as this oil naturally contains low levels of CBD, which is considered a non-psychoactive compound. This applies to CDB oil obtained by cold-pressing the hemp seeds. If and when the oil is obtained by supercritical CO2 extraction, then a Novel Food authorization is mandatory.
Denmark: available guidance not crystal clear
According to the Danish Ministry of Environment and Food, a number of Cannabis-derived products are not considered Novel Food, notably hemp seeds, seed flour, protein powder from seeds and seed oil from the Cannabis sativa L. varieties listed in the EC Plant Variety Database that are free from or contain low levels of THC. If these products contain CBD, the regulatory status is not exactly clear. According to the guidance of the Danish Food Ministry, the current status is that pure cannabidiol as well as hemp products with high (concentrated) levels of CBD or other cannabinoids are covered by the Novel Foods Regulation. It is not explained what is understood by “high levels of CBD”, but on the other hand an absolute prohibition to market these products in Denmark does not seem to apply.
Absolute prohibitions: Belgium and Austria
Other Member States seem to be stricter than Ireland or Denmark. For instance, the Austrian Health Ministry has made it perfectly clear that food products containing any type of cannabinoid extract without a Novel Food authorization are prohibited to be put on the market. In Belgium, the Federal Agency on Safety in the Food Chain has clarified that the production and marketing of food products based on cannabis is prohibited. The rationale is that the plant Cannabis sativa is mentioned in an annex to a national Decree listing dangerous plants that cannot be used for food production. The prohibition primarily seems to target the potentially dangerous substance of THC and allows derogations on a case-by-case basis, but not regarding food products containing CBD. These are considered Novel Foods requiring a market authorization.
Enforcement directed against (medical) claims in the Netherlands
Until CBD was declared a Novel Food, the trade in CBD food products was not prohibited in the Netherlands. Contrary to the substance TCH, the substance CBD is not mentioned in the Dutch Opium Act, listing prohibited substances having a psycho active effect. This does not mean that the trade in CBD food products was allowed just like that. In practice, enforcement in the Netherlands has been directed against the use of any unauthorized medical claims. A medical claim is any information according to which a food product could have a therapeutic or prophylactic effect. When using such a claim, one comes into the realm of the Medicinal Product Act, according to which it is prohibited to market and advertise any medicinal product without a market authorization. The Dutch Food Safety Authority announced fines up to
€ 10.000 regarding the sale of CBD food products in several cases (see here and here). Any food business operator that is serious about his business in CBD food products will therefore not only check the applicability of the Novel Foods Regulation to his products, but also carefully draft his advertisement for this type of product.
Conclusion
The production and marketing of food products derived from Cannabis sativa L. in the EU has been considerably restricted since CDB food products were recently declared to be Novel Foods. However, not all cannabis-derived food products require market authorization. Pending the evaluation of the Novel Food application filed for a CBD food supplement by the Czech company Cannabis Pharma, it is worthwhile for other CBD food products to verify whether they can benefit from the so-called transition regime embodied in the Novel Foods Regulation. Due to differences between legislation in the Member States, this may differ from country to country. Also, it is important to carefully position your CBD food product, in order to avoid any medical claims.
The author ackowledges Jasmin Buijs, paralegal at Axon, and Max Luijkx, intern at Axon, for their valuable input.
Posted: July 16, 2018 | Author: Karin Verzijden | Filed under: Authors, Enforcement, Food, Health claims, Nutrition claims |
 Last week, the creation of the new Advisory Group on the Status of Borderline Products was published in the Dutch Government Gazette. The Advisory Group consists of expert representatives from the Healthcare Inspectorate, the Food Safety Authority, the Medicines Evaluation Board and the Central Committee on Research Involving Human Subjects. Its task is to issue advice on the legislation to be applied to individual products / product groups / substances belonging to a group of so-called borderline products. The reason that this Advisory Group was created is that the regulations in the field of market authorization and research with such products are complex and that it is not always clear which law is applicable. In such case it is also not clear which enforcement authority is competent to act in case of violations of the law. This is deemed undesirable by both the marketplace and the government authorities and the Advisory Group aims to change this.
Last week, the creation of the new Advisory Group on the Status of Borderline Products was published in the Dutch Government Gazette. The Advisory Group consists of expert representatives from the Healthcare Inspectorate, the Food Safety Authority, the Medicines Evaluation Board and the Central Committee on Research Involving Human Subjects. Its task is to issue advice on the legislation to be applied to individual products / product groups / substances belonging to a group of so-called borderline products. The reason that this Advisory Group was created is that the regulations in the field of market authorization and research with such products are complex and that it is not always clear which law is applicable. In such case it is also not clear which enforcement authority is competent to act in case of violations of the law. This is deemed undesirable by both the marketplace and the government authorities and the Advisory Group aims to change this.
Demarcation issues not new
Demarcation issues at the interface of the laws applicable to food products and medicinal products are not new. Already in a 2008 Letter to Parliament, the Dutch Health Minister reported that there was insufficient clarity about the demarcation between medicinal products and herbal remedies. The Minister reported the issue that a herbal remedy could also be a medicinal product within the meaning of the Dutch Act of Medicinal Products (in which the Medicinal Products Directive 2001/83 has been implemented). This is a consequence of the fact that the Act does not make a distinction between the origin of any active substance, which can be of human, animal, vegetable or chemical origin. When a herbal preparation qualifies as a medicinal product by function or by presentation, the Act on Medicinal Products is equally applicable.
Measures announced in the Letter of Parliament
At the time, the Health Minister did not consider it necessary to adjust the regulations to prevent demarcation issues between food products and medicinal products. He considered the criteria of “medicinal product by presentation” and “medicinal product by function” to be sufficiently clear in the first place. Secondly, he expected a beneficial effect from the list of permitted health claims that still had to be published back in 2008. He anticipated that products bearing such claims would not qualify as a medicinal product by presentation. He did, however, consider it desirable to improve cooperation between the Heath Care Inspectorate and the Food Safety Authority. This was implemented by adjusting the Decree on Supervision of Public Health, as a result of which the Food Safety Authority gained authority to enforce violations of the Act on Medicinal Products. Furthermore, it was stipulated that the structured consultation between the Heath Care Inspectorate, the Food Safety Authority and the Medicines Evaluation Board should be intensified, particularly regarding the discussion of the status of borderline products. One can say that this consultation in fact operated as an Advisory Group avant la lettre. Finally, it was determined that the already existing cooperation agreement between the Heath Care Inspectorate and Food Safety Authority had to be updated.
Demarcation issues more topical than ever
We now know that the clarification brought by the list of authorized health claims published in 2012 should not be overestimated. Nowadays many functional foods and nutraceuticals are marketed that claim medical properties. It quite often happens that it is not clear what is the applicable legislation to these products, because the boundary between health claims, disease risk reduction claims and medical claims is not immediately clear in all cases. Even when no specific claim is used, it can be debatable whether a product is a medicinal product by function or any other health product. It also happens that more or less the same products are marketed simultaneously as a medicinal product and as a foodstuff. Consider, for example, products containing glucosamine or St. John’s Wort. This means that food products containing the same active substance as medicinal products have not passed the prior testing for quality, safety and efficacy, which can be confusing for the consumer.
Consequences of product qualification
There are many examples of food products that were considered medicinal products by presentation. Consider, for example, the melatonin products which, after a remarkable turn in the Health Care Inspectorate policy, initially not but later on were considered to be medicinal products. More recently, a medical claim that Milk Thistle could prevent liver fattening was considered misleading. Furthermore, it was determined that a dietary supplement that would promote the natural immune system, would have a beneficial effect on heart and blood vessels and would help to treat fatigue qualified as a medicinal product. When such disputes are dealt with before the Civil Court, quite often fines are imposed for violations of the Act on Medicinal Products, prohibiting, among other things, the marketing and advertising of medicinal product without a marketing authorization. When these disputes are submitted to the Advertising Code Committee, usually a recommendation is made to no longer use such misleading information based on these regulations and the Code on Public Advertising of Medicinal Products. In order to prevent such enforcement activities, manufacturers of health products have every interest in knowing in advance how their product qualifies. They then know which regime applies to their product and can take this into account in their communication (advertising campaigns).
Working method Advisory Group
How does the Advisory Group work and which aspects are covered by its advice? Upon request of one of the competent authorities, the Advisory Group advises on the applicable legislation to individual products, product groups or substances. This advice gives a motivated indication of the law that applies to the opinion of the Advisory Group at the time of assessment and given the available information. “Available information” refers not only to factual information but also to applicable case law, both in the Netherlands and abroad. The advice will be presented to the Healthcare Inspectorate, the Food Safety Authority, the Medicines Evaluation Board and the Central Committee on Research Involving Human Subjects, who will subsequently respond to this within four weeks if so desired. If the responses give cause to do so, the Advisory Group reconsiders the advice and if necessary adjusts it. The advice is then recorded in its database, which is managed by its secretariat. There is also a possibility that the Advisory Council will not reach agreement on the applicable legislation. In such a case no advice is issued; this is also recorded in the database. The Advisory Group can also change its advice in the event of changes in the legal framework. The competent enforcement authorities must report those change to the Advisory Group, which registers an amendment to a previous advice in its database, if and when applicable. For clarity, the advice assesses neither the efficacy, safety or efficacy of medical products nor the content of any research protocols.
Added value Advisory Group
Can it be expected that the Advisory Group will make a substantial contribution to demarcation issues? In itself, the intensified co-operation between all the authorities involved, at market entry rather than upon enforcement during marketing, is to be welcomed. For example, in practice, food business operators also benefit from the working agreements between the Council on Advertising Health Products and the Food Safety Authority, on the basis of which health products bearing a “stamp” of said Council are in principle not exposed to enforcement actions by the Food Safety Authority. However, it appears from the currently published agreement between the parties involved in the Advice Group that only the enforcement authorities and not the individual manufacturers can request advice from the Advisory Group. This appears to be a missed opportunity, as is the fact that the efficacy of medicinal products remains explicitly outside the Advisory Council’s assessment. To qualify the essential character of a health product, efficacy is one of the essential factors. Furthermore, it is noteworthy that the Advisory Group does not seem to address the issue of medical devices, while this qualification is closely linked to that of medicinal or food products. For example, cranberry pills against bladder infection qualify as medical devices and osmotic laxatives can be either medicinal products or medical devices.
Advice on market access for health products
For the time being, manufacturers of health products will continue to rely on private advice from qualified advisors on market access for health products. Nevertheless, the body of opinions to be produced by the Advice Group can be a valuable source of information, provided that its database will be publicly searchable. The rules of procedure of the Advice Group, which are yet to be made available, will have to provide clarity in this respect.
Posted: July 31, 2017 | Author: Karin Verzijden | Filed under: Authors, Enforcement, Food, Information |
 The European Court of Justice (ECJ) recently took its decision in the TofuTown case, providing clarity on the interpretation of the Agricultural Product Standards Regulation (APS Regulation). In short, this case dealt with the question: “Is it possible to use regulated product names for new product types?” The answer to this question is a clear “no”. This came as quite a shock to the emerging vegetarian and vegan market. Many companies marketing alternative protein products use traditional product names for their dairy replacements. They may have to change these names, as they are no longer in line with the view of the highest EU Court.
The European Court of Justice (ECJ) recently took its decision in the TofuTown case, providing clarity on the interpretation of the Agricultural Product Standards Regulation (APS Regulation). In short, this case dealt with the question: “Is it possible to use regulated product names for new product types?” The answer to this question is a clear “no”. This came as quite a shock to the emerging vegetarian and vegan market. Many companies marketing alternative protein products use traditional product names for their dairy replacements. They may have to change these names, as they are no longer in line with the view of the highest EU Court.
Initiator: Verband Sozialer Wettbewerb
The TofuTown case was initiated by the German unfair competition association Verband Sozialer Wettbewerb (“VSW”). This activist organisation was also at the origin of the Innova Vital case, clarifying the scope of the EU Claims Regulation. Based on this decision, we now know that the Claims Regulations not only targets commercial communications addressing final consumers, but under certain circumstances, it also addresses communications made to health care professionals. VSW initiated the present case against the German company TofuTown, as it claimed the promotion of strictly plant-based products under denominations such as “Soyatoo Tofubutter”, “Pflanzenkäse” and “Veggiecheese” infringed the EU competition rules.
Main rule of Agricultural Product Standards Regulation
The legal framework of this dispute is constituted by the APS Regulation, containing detailed agricultural products definitions in various sectors, such as cereals, olive oil, wine, milk and milk products. The main rule following from the APS Regulation is that the names of regulated products may not be used for other products. TofuTown had argued, in essence, that this principle is outdated. In the past, such rule may have been justified to protect consumers against manufacturers distributing cheap products as dairy products, thereby gaining a competitive advantage. Nowadays, consumer awareness has changed considerably and many consumers want to be informed about alternatives to dairy products. Using regulated dairy names for plant-based alternatives is not meant to mislead consumers. Quite to the contrary, such use enables to inform the consumer on plant-based origin of their products as opposed to the animal derived dairy products they intend to replace. The ECJ did not agree with this argument. It is nevertheless worthwhile to investigate if any other argument could escape the strict product name regime embodied in the APS Regulation.
Room for manoeuvre in APS framework?
On the face of it, there is. The Commission is empowered to adopt delegated acts concerning exemptions to the strict product definitions laid down in the APS Regulation, provided these shall be strictly limited to demonstrated needs resulting from evolving consumer demand, technical progress or the need for product innovation (see article 78.3 APS Regulation). Tofutown’s plea for informing consumers about plant-based alternatives to dairy products seems to fit in seamlessly in this derogation. However, for the time being, there is no such delegated act, so that it is worth while exploring if there any further exceptions to the strict product names principle embodied in the APS Regulation.
Composite products
In fact, two of these exceptions are being mentioned in the TofuTown case. In the first place, designations for milk products may also be used in association with words designating composite products. The condition precedent is that no part takes the place of any milk constituent. Furthermore, milk should also be the essential part of such composite product, either in terms of quantity or for the characterisation (see Annex VII belonging to the APS Regulation, in particular Part III, nr. 3 thereof). An examples of such composite product names is chocolate milk.
Traditional usage
Another exception to the system of strict product names relates in the first place to products the exact nature of which is clear from traditional usage. In the second place it covers designations that are clearly used to describe a characteristic quality of the product. The Commission has drawn up a limitative list of such product names that can be found here. Examples of such product names are the following:
- UK: horseradisch cream, cream crackers and coconut milk
- France: almond milk (lait d’amande) and oat cream (crême d’avoine)
- Spain: almond milk (leche de almendras)
- Netherlands: butter beans (boter bonen) and cacao butter (cacao boter)
This list has a highly cultural character and does not allow for translations of the product names mentioned therein into other Member States languages. As such, it would be prohibited to market almond milk in or any other EU country than France and Spain. The same goes for butter beans outside the Netherlands.
Practical consequences
It could be argued that names like “Tofubutter” and “Veggiecheese” are clearly used to describe a characteristic quality of the product. However, as long as they are not mentioned on the Commission exemption list, these cannot be legally used for marketing plant-based alternatives to dairy products. More in general, the practical consequences of the TofuTown decision are expected to bring about serious restrictions for marketing plant-based products. Is this to be considered a setback for the consumer or to the contrary, will this prevent any consumers being misled? In fact, this is besides the point, as based on this decision, the enforcement authorities, like the Dutch Food Safety Authority (“NVWA”) in the Netherlands, will be authorised to prohibit further use of strictly regulated product names for their vegetarian peers. It will be interesting to see though if any enforcement actions will take place based on the mere product name. And also, will this be in the interest of the educated consumers of today? That’s certainly not beside the point.
Posted: December 7, 2016 | Author: Karin Verzijden | Filed under: Authors, Enforcement, Food, Health claims, Information, Nutrition claims |
 On 24 November last, the Dutch Life Sciences Conference took place in Leiden, the Netherlands. This conference brings together a large number of life sciences professionals from the Netherlands and abroad. One of this year’s sessions was dedicated to cross sector innovations, during which DSM, NutriLeads, i-Optics and Axon Lawyers shared their take on this topic. This post captures the legal presentation made during this session on cross over innovations, focussing on the applicable rules to borderline products. These rules are explained on the basis of landmark ECJ decisions and recent Dutch case law. The slides belonging thereto can be viewed here.
On 24 November last, the Dutch Life Sciences Conference took place in Leiden, the Netherlands. This conference brings together a large number of life sciences professionals from the Netherlands and abroad. One of this year’s sessions was dedicated to cross sector innovations, during which DSM, NutriLeads, i-Optics and Axon Lawyers shared their take on this topic. This post captures the legal presentation made during this session on cross over innovations, focussing on the applicable rules to borderline products. These rules are explained on the basis of landmark ECJ decisions and recent Dutch case law. The slides belonging thereto can be viewed here.
Product qualification
In order to demonstrate that it is not always easy to correctly qualify life sciences products, a few decisions from Dutch Courts and the Advertising Code Committee were discussed (see slides 3 – 7). According to a recent decision of the Dutch Supreme Court in the field of tax law, toothpaste and sun cream were surprisingly qualified as medicinal products. This case had been initiated in 2010 by two drugstores that were unhappy they had to pay the regular VAT rate of 21 % with respect to these products. According to the drugstores, these products qualified as medicinal products, to which a VAT rate of 6 % is applicable. Although their plea had been dismissed in two instances, the Supreme Court agreed with the drugstores that based on the presentation criterion (see below), both products indeed qualified as medicinal products, as they advertised therapeutic or prophylactic effects. With respect to toothpaste, this was due to the natrium fluoride protecting against caries and with respect to sun cream, the UVA and UVB filters were supposed to protect the skin against sunburn.
Legal framework
The case discussed above so far stands in isolation, but here are many cases that have shed light on the distinction between two categories of life sciences products, being food and medicinal products. Below you will find 5 criteria that will help you to apply this distinction. In slides 8 – 12, you will find the applicable legal sources.
- The legal product definitions should be taken as a starting point. Bottom line, medicinal products are products aimed curing, prevention or diagnosis of a disease, whereas food products are products intended to be ingested by humans.
- A distinction is being made between medicinal products by presentation and medicinal products by function. Extensive case law is available for the interpretations of these notions (see below). In case of doubt, the rules relating to medicinal products shall prevail.
- It is prohibited to advertise medicinal products without having a market authorisation. For advertising of food products, it is permitted to use authorised health claims, but it is prohibited to use medical claims.
- Medical claims are communications claiming that the advertised products improve health problems. It is a thin line between non-authorised medical claims and authorised disease risk reduction claims.
- The notion of advertising can be pretty broad. According to the Dutch Advertising Code it comprises any public and/or systematic direct or indirect recommendation of goods, services or views for the benefit of an advertiser, whether or not using third parties.
Medicinal Products by presentation
In the landmark ECJ case Van Bennekom, the presentation criterion to qualify medicinal products was introduced. The case related to a Dutch national, who was caught with large quantities of vitamin preparations for medicinal purposes in pharmaceutical form, however without any required pharmaceutical authorisations. Van Bennekom did not deny the facts, but he alleged that he was not marketing medicinal products, but food products. The ECJ ruled that for the sake of consumer protection, the presentation criterion not only covers products having a genuine therapeutic or medical effect but also those regarding which consumers are entitled to expect they have such effect. In sum, the presentation criterium should be broadly interpreted on a case-by-case basis, taking into account all relevant factors. The concentration level of active ingredients forms only one of those factors.
Medicinal products by function
The ECJ Hecht-Pharma decision is still leading to set the parameters to decide if a product qualifies as a medicinal product by function. Hecht Pharma was marketing in Germany a fermented rice product in the form of capsules presented as being food supplements. Further marketing was prohibited, as the product contained significant levels of monalin k, which is an inhibitor of cholesterol synthesis. The product was considered as a medicinal product by function, for the marketing of which a market authorisation would be required. The ECJ ruled in this case that for the purposes of deciding if a product falls within the definition of medicinal product by function, the national courts must decide on a case-by-case basis, taking into account all characteristics of the product, such as its composition, its pharmacological properties and manner of use, the extent of its distribution, its familiarity to consumers and the risks, which its use may entail. As reported in a recent post, these criteria are still valid.
Functional foods
A recent Dutch decision on a licensing dispute entailed so-called functional foods. Although this notion does not have a legal definition under EU standards, it is usually understood as food having certain medicinal properties. The dispute divided Unilever and Ablynx, who both had obtained a license from the Brussels University (VUB) under certain antibody patents owned by VUB. Unilever’s licensed related to (roughly speaking) food products, whereas Ablynx’ license related to medicinal products. Under its license, Unilever developed so-called functional foods having certain beneficial effects against infections caused by the rotavirus. Ablynx claimed that Unilever had thus operated outside its licensed field and thereby acted unlawfully vis-à-vis Ablynx. The Hague Appeal Court endorsed Ablynx’ claims, on the assumption that Unilever’s license was clearly directed against non-pharmaceutical products. As such, it could target general health benefits (such as lowering cholesterol), but not specific pathogens.
Take home
What can you learn from the above? It is important to obtain pre-market clearance for the communication on health products. For this purpose, you can take guidance from the Advertising Code on Health Products (Code aanprijzing gezondheidsproducten), applicable to products having a pharmaceutical form and a health related primary function, however without being medicinal products. You could also request pre-market clearance from KOAG-KAG, whom actively evaluates claims on health products and provide endorsements. If and when you are confronted with enforcement measures by either the Dutch Health Care Inspectorate (Inspectie Gezondheidszorg or IGZ) or the Dutch Food Safety Authority (Nederlandse Voedsel en Waren Autoriteit or NVWA), first try to buy some time by claiming an extension for response. Subsequently, carefully consider if the claims made by the enforcement authorities are factually correct and legally enforceable. Whenever helpful or necessary, obtain professional support.
Posted: November 9, 2016 | Author: Sofie van der Meulen | Filed under: Disclosure of information, Enforcement, Food | Tags: disclosure, enforcement, inspection, NVWA |
 Recently, an amendment to the Dutch Health Act (Gezondheidswet) was voted in Dutch Parliament, allowing the Dutch Food Safety Authority (Nederlandse Voedsel en Warenautoriteit or NVWA) to actively disclose its inspection results. The change in the Health Act equally applies to inspection results obtained by the Dutch Health Inspectorate (Inspectie Gezondheidszorg or IGZ) and therefore, it received broad interest from the pharmaceutical, medical devices, and the food industry and their legal practitioners. Three meetings on this topics were organised by respectively the Dutch association of Food Law (NVLR), the Dutch Pharmaceutical Law Association (VFenR) and by the Dutch organisation for food retail and management VMT. This post will put you up to speed on the actual changes to be applied to the Health Act, as well as on the expected consequences of their implementation for food business operators (FBOs).
Recently, an amendment to the Dutch Health Act (Gezondheidswet) was voted in Dutch Parliament, allowing the Dutch Food Safety Authority (Nederlandse Voedsel en Warenautoriteit or NVWA) to actively disclose its inspection results. The change in the Health Act equally applies to inspection results obtained by the Dutch Health Inspectorate (Inspectie Gezondheidszorg or IGZ) and therefore, it received broad interest from the pharmaceutical, medical devices, and the food industry and their legal practitioners. Three meetings on this topics were organised by respectively the Dutch association of Food Law (NVLR), the Dutch Pharmaceutical Law Association (VFenR) and by the Dutch organisation for food retail and management VMT. This post will put you up to speed on the actual changes to be applied to the Health Act, as well as on the expected consequences of their implementation for food business operators (FBOs).
Importance of inspection results
Inspection results are important for whom it concerns directly (inspected companies, as they provide answers to questions such as: is your organisation compliant? Will a fine be imposed? Inspection results are furthermore of interest to others, such as consumers, journalists and other companies, including competitors, for a number of reasons. These reasons include (but are not limited to) knowing where to supply from and what places to avoid, the possibility to check if your supplier’s manufacturing processes are up to standards and the option to stay informed on what challenges your competitor is meeting.
Active vs. passive disclosure
All administrative bodies disclose information, on their website, in social media, in leaflets, etc. Under the Dutch Act on Public Access to Government Information (Wet openbaarheid van bestuur or WOB) citizens have the right to file a request for information on administrative matters. The disclosure of such information on request of a person is called passive disclosure. Such disclosure does not take place publicly, but the information concerned will solely be provided to the person who filed the request, unless it is rejected based on the limited grounds specified in the WOB. Active disclosure on the other hand means that the information is disclosed by an administrative body prior to any request for information. Such information is publicly available after disclosure. In case of inspection results of the NVWA, these will most likely be published on the website this administrative body.
Rationale disclosure inspection results
The rationale for both passive and active disclosure of inspection results is threefold.
(i) Transparency. Without information on the inspection, one cannot assess the quality of the inspection or view the results of the inspection. This transparency is also present in other areas such as inspection results of the Inspectorate of Education and the Health Care Inspectorate.
(ii) Trust. By showing the results, the public can see what the NVWA is doing and therefore the public can build trust in the NVWA.
(iii) Increased compliance. Negative results of an inspection can lead to serious problems towards consumers or customers, such as liability claims from suppliers who expected to be supplied with products produced in compliance with the applicable quality standards and hygiene regulations). In this way active disclosure increases the pressure on FBOs to comply.
The current system
Opposed to other inspectorates in the Netherlands, the active disclosure by the NVWA is currently not provided for in a specific Act. So far, the mechanism laid down in the WOB has been used as the framework for disclosure of inspection results. Article 8 WOB enables the NVWA to actively disclose information, provided this is done is a clearly understandable way and offering interested parties in due time the opportunity to comment. As far as a request for information by any company or citizen is concerned, there are predefined grounds on which an administrative body cannot freely disclose information, being absolute and relative grounds. The absolute grounds are found to be of such importance that publication is interdicted, like confidential commercial information relating to the safety of the state or information containing personal data. The relative grounds relate for instance to privacy matters or to disproportional harm that could be created by publication. Such grounds have to be weighed against the interests of disclosure. In the current framework, the interested party can express a provisional opinion with respect to any intended publication by NVWA, which has to be dealt with before publication. This mechanism will disappear under the new system.
The new system
When the amendment of the Health Act will enter into force, the NVWA will not only have the option to actively disclose information, but will be obliged to do so. In the legal framework, the assessment of interests is already taken into account, which makes it unnecessary to do another assessment each time the NVWA decides to actively disclose information. In future, the option to express a provisional opinion by the NVWA will no longer be available. The only way to ensure that the information is not disclosed is starting summary proceedings before a civil court. If any interested party is doing so, NVWA will then be forced to suspend its decision to disclose information until the court decides on the matter. In case the NVWA will disclose the inspection report, the NVWA will provide the option for FBOs to provide a reaction to the inspection results, which will be disclosed together with the inspection results. In addition to the change applied to the Health Act, an underlying decree needs to specify more detailed rules on what information exactly needs to be published in what format. In the discussions on the amendment of the Health Act another amendment was added which ensures the underlying decree can only be amended with the approval of Dutch Parliament.
Current status of the amendment
On the 11th of October the House of Representatives of the Netherlands (Tweede Kamer) accepted the proposed changes to the Health Act and amended some parts. The Dutch Senate (Eerste Kamer) accepted the amendments without making any additional amendments on the 1th of November. However, the change of the Health Act has not yet entered into force and it is currently still unclear when the exact date of entry into force will be. Guestimates are hinting at June 2017, however the Ministry of Health Welfare and Sport is still working on the underlying decree on what information has to be published and in what format. There is a fair chance the amendment will only enter into force simultaneously with this underlying decree. In such case the entry into force of the changes to the Health Act will most likely be later than the guestimate mentioned above.
Situation in other EU countries and NVWA pilot
Other EU Member States already have a system of active disclosure of inspection results for restaurants in using a system of easily understandable designations or colours (Denmark and Ireland for instance). In those countries, the outcome of the inspection is presented at the entrance of the inspected restaurant, in order to give the public an overview of the level of compliance at first glance. For instance, a green colour or a happy face means that the restaurant is compliant and colours closer to red or a less happy face mean the place was less compliant. In the Netherlands, the NVWA launched a pilot for disclosure of inspection results for lunchrooms, which were disclosed via an app. This app subsequently displayed the results on a map. The map showed the lunchrooms in four different colours, depending on the level of compliance. The idea was to provide a quick overview of the lunchrooms and the level of compliance. However, the reaction of the minister of Health, Welfare and Sport to this format was negative due to interpretation issues, particularly interpretation of the colours. There are also lists of inspected products instead of inspected FBOs. The experience gained therewith and during the pilot will have to be evaluated in order to choose an acceptable form for the disclosure of over 200.000 inspections done each year in the Netherlands by the NVWA.
Criticism
The proposed changes to the Health Act have been much criticised. The active disclosure of the inspection results together with the imposed sanctions can be viewed as punitive sanction in addition to the sanction itself imposed based on the findings during the inspection. In the explanatory notes on the amendment of the Health Act, the government explains that active disclosure should not be perceived as a punitive sanction and therefore not a criminal charge in the sense of Art. 6 ECHR. In case the disclosure will be viewed as a punitive sanction, article 6 ECHR will be applicable, meaning the procedural safeguards embodied in this article will apply. Basically, the government states that the disclosure does not aim at punishing the inspected party, and therefore is not an additional sanction. However, the arguments provided by the government in the explanatory notes are not very convincing. Assuming the disclosure will lead to more transparency, consumers and customers will be aware of the non-compliance due to the disclosure. This disclosure can in turn decrease the trust in the non-compliant producer, which could mean a decline in sales or even liability claims from consumers or customers. It is not the fines imposed by the NVWA, but the disclosure of the inspection results, which leads to these (potential) damages of the producer, whom will not have had the chance to remedy the situation before it is out in the open. This is all the more important, as so far there is no evidence that such public disclosure indeed will lead to an increased level of compliance. Moreover, this situation does not seem to be in line with competition law, which constitutes the regular level playing field of any FBO, just like it is for manufacturers of medical devices or medicinal products. Therefore, competition law elements should in our opinion be an aspect of the legislation concerning disclosure. In the explanatory notes to the amendment, this aspect has not even been mentioned.
Conclusion
As a result of a change applied to the Dutch Health Act, the first steps towards active disclosure of inspection results from the NVWA have been initiated. The actual implementation thereof depends on the underlying decree, which is still under construction. This is why is not clear as of when the legal basis for active disclosure of NVWA inspection results will be operational. As of this moment however, FBOs will be subject to increased enforcement measures, without the effect thereof being necessarily positive. We will keep an eye out for you and report on any relevant development in this field, as they are likely to have an important impact for each FBO.
The author thanks Floris Kets for his contribution to this post.
 In principle, a medicinal product cannot be sold in the Netherlands without an authorization. Advertising a medicinal product that has not been authorized is prohibited as well. If a product is classified as such and sold without a license, the seller risks a hefty fine.
In principle, a medicinal product cannot be sold in the Netherlands without an authorization. Advertising a medicinal product that has not been authorized is prohibited as well. If a product is classified as such and sold without a license, the seller risks a hefty fine. The court agreed with this argumentation, referring to the amendment of the Medicinal Product Directive of 2004. The court deduces from the preamble to the amendment that the Medicinal Product Directive does not apply if there is no doubt that a product clearly exclusively belongs to another product category, such as food or food supplements. The court ruled that this was indeed the case for the specific circumstances that were under discussion. The products clearly fall under the category of food supplements and therefore solely food law applies. The court confirms that the Dutch Medicines Act must, after all, be interpreted in accordance with the Medicinal Product Directive. The court therefore does not proceed testing the medical claims made against the presentation criterion based on drug legislation at all.
The court agreed with this argumentation, referring to the amendment of the Medicinal Product Directive of 2004. The court deduces from the preamble to the amendment that the Medicinal Product Directive does not apply if there is no doubt that a product clearly exclusively belongs to another product category, such as food or food supplements. The court ruled that this was indeed the case for the specific circumstances that were under discussion. The products clearly fall under the category of food supplements and therefore solely food law applies. The court confirms that the Dutch Medicines Act must, after all, be interpreted in accordance with the Medicinal Product Directive. The court therefore does not proceed testing the medical claims made against the presentation criterion based on drug legislation at all. Recently, an amendment to the Dutch Health Act (Gezondheidswet) was voted in Dutch Parliament, allowing the Dutch Food Safety Authority (Nederlandse Voedsel en Warenautoriteit or NVWA) to actively disclose its inspection results. The change in the Health Act equally applies to inspection results obtained by the Dutch Health Inspectorate (Inspectie Gezondheidszorg or IGZ) and therefore, it received broad interest from the pharmaceutical, medical devices, and the food industry and their legal practitioners. Three meetings on this topics were organised by respectively the Dutch association of Food Law (NVLR), the Dutch Pharmaceutical Law Association (VFenR) and by the Dutch organisation for food retail and management VMT. This post will put you up to speed on the actual changes to be applied to the Health Act, as well as on the expected consequences of their implementation for food business operators (FBOs).
Recently, an amendment to the Dutch Health Act (Gezondheidswet) was voted in Dutch Parliament, allowing the Dutch Food Safety Authority (Nederlandse Voedsel en Warenautoriteit or NVWA) to actively disclose its inspection results. The change in the Health Act equally applies to inspection results obtained by the Dutch Health Inspectorate (Inspectie Gezondheidszorg or IGZ) and therefore, it received broad interest from the pharmaceutical, medical devices, and the food industry and their legal practitioners. Three meetings on this topics were organised by respectively the Dutch association of Food Law (NVLR), the Dutch Pharmaceutical Law Association (VFenR) and by the Dutch organisation for food retail and management VMT. This post will put you up to speed on the actual changes to be applied to the Health Act, as well as on the expected consequences of their implementation for food business operators (FBOs).